Society
Today 5:00 am
Will the Opioid Crisis Deliver Its Worst Harms to Black and Brown People?
Will the Opioid Crisis Deliver Its Worst Harms to Black and Brown People?
It started as a crisis among white people. But now that overdoses are surging in Black and Brown communities, government is failing to invest in the healthcare-based approaches that we know would save lives.
August 28, 2023
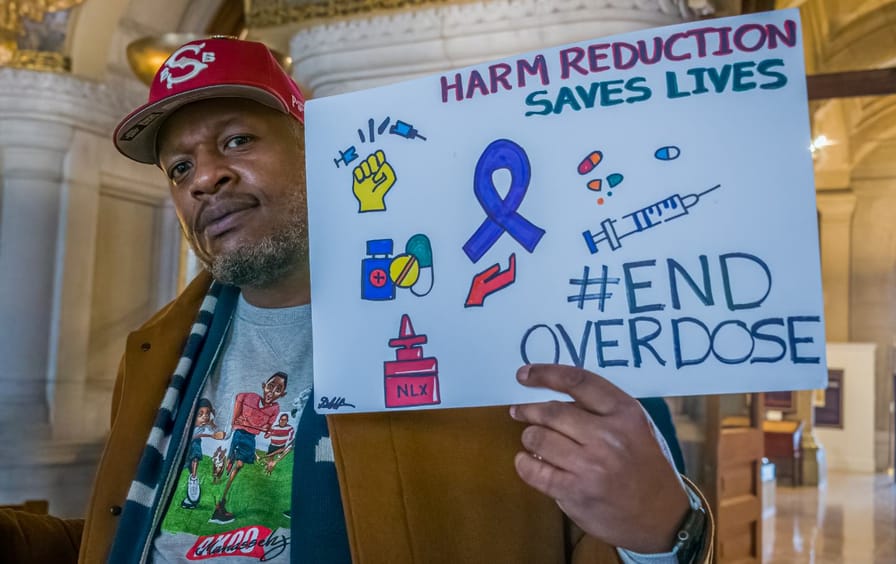
Advocates protested in Albany, N.Y., against the criminalization of opioid users in the state. (Erik McGregor / LightRocket via Getty Images)
Subscribe to The Nation
Subscribe now for as little as $2 a month!
Get The Nation’s Weekly Newsletter
Fridays. The best of the week.
By signing up, you confirm that you are over the age of 16 and agree to receive occasional promotional offers for programs that support The Nation’s journalism. You can read our Privacy Policy here.
Repro Nation
A monthly newsletter on the global fight for reproductive freedom.
By signing up, you confirm that you are over the age of 16 and agree to receive occasional promotional offers for programs that support The Nation’s journalism. You can read our Privacy Policy here.
Subscribe to The Nation
Subscribe now for as little as $2 a month!
Support Progressive Journalism
The Nation is reader supported: Chip in $10 or more to help us continue to write about the issues that matter.
Sign up for our Wine Club today.
Did you know you can support The Nation by drinking wine?
In America today, while the “opioid crisis” is still commonly associated with white people, overdose deaths are increasing the fastest in Black and brown communities. As the overdose rate climbs, government at all levels has been far slow to implement strategies that we already know can reduce harms. It raises a haunting historical specter: Will overdoses be one more white crisis that ultimately delivers the worst harms to Black and brown people?
The white origins of the opioid crisis are well known. Beginning in the 1990s, Purdue Pharma and its many competitors flooded white rural and suburban communities, especially in the Northeast, Appalachia, and the upper Midwest, with newly patented pain pills deemed “minimally addictive” by the FDA. The easy access to opioids among both adults and youth in these communities contributed to skyrocketing rates of addiction and, ultimately, overdose.
Rather than arresting the users, authorities concerned about opioid deaths of ”suburban youth” (coded language for young white people) instead focused on preventing prescribers and pharmacists from giving opioid “abusers” access to pharmaceutical opioids. State governments implemented Prescription Drug Monitoring Programs to identify and reject ”doctor shoppers,” and physicians or pharmacists who catered to them were criminally prosecuted. Meanwhile, opioid manufacturers developed tamper-resistant formulations that made it more difficult to snort or inject their products (and that extended the profitability of the newly patented formulations against the generic competitors that had emerged for their original product).
What this did not take into consideration was that a generation of white suburban “abusers,” now banished from accurately labeled and quality-controlled pharmaceutical grade opioids, were forced to switch to totally unregulated heroin markets.
This article is adapted from the authors’ new book, Whiteout: How Racial Capitalism Changed the Color of Opioids in America.
Prohibition markets—that is, markets governed only by criminalization rather than consumer protections—for heroin had been well entrenched in American cities for nearly a century. Consumers in these markets were harshly policed, often incarcerated, and faced devastating collateral consequences, social stigma, and personal risks, but they did not die from heroin overdose in the numbers we have seen in recent decades—it may not have been easy, but most consumers survived these markets. The sudden influx of former prescription opioid consumers in early the 2000s disrupted that delicate ecosystem, drawing in new suppliers and intensifying competition and innovation. This eventually led drug cartels to switch to more potent and thus easier to smuggle drugs, in this case, fentanyl instead of heroin. (A century before, a similar prohibition-era ban on smoking opium led dealers to switch to heroin.)
Although the shift to fentanyl happened because of the surge of white opioid consumers, everyone has to contend with it. This includes the Black and brown neighborhoods where heroin markets had settled into recognizable patterns and products that allowed consumers to make safer choices. As Black and brown heroin consumers became Black and brown fentanyl consumers, however, those strategies worked less well, and overdose rates climbed.
Popular
“swipe left below to view more authors”Swipe →
Undercover With the New Alt-Right
Undercover With the New Alt-Right
Republicans Are Wrong on Abortion—and They Know It
Republicans Are Wrong on Abortion—and They Know It
We Are Witnessing the First Stages of Civilization’s Collapse
We Are Witnessing the First Stages of Civilization’s Collapse
Nora Ephron’s Divorce Plot
Nora Ephron’s Divorce Plot
Popular
“swipe left below to view more authors”Swipe →
Undercover With the New Alt-Right
Undercover With the New Alt-Right
Republicans Are Wrong on Abortion—and They Know It
Republicans Are Wrong on Abortion—and They Know It
We Are Witnessing the First Stages of Civilization’s Collapse
We Are Witnessing the First Stages of Civilization’s Collapse
Nora Ephron’s Divorce Plot
Nora Ephron’s Divorce Plot
As the pharmaceutical opioid addiction crisis shifted into an opioid overdose crisis, authorities and health departments crafted a new health care–based, rather than punitive, approach to addiction for the newly recognized population of prescription opioid “abusers,” most prominently featuring increased treatment and, especially, medication assisted treatment. These new policies were implicitly and explicitly billed as ways to rescue white people, and this was easily seen in their implementation. For example, according to a 2019 study published in JAMA Psychiatry, buprenorphine, a long-acting opioid that could be prescribed in regular medical practice to stabilize and regularize consumption, is overwhelmingly prescribed to white people. Black and brown people mostly had access to the chemically similar but older and punitively policed methadone. Public health departments began investing in harm reduction strategies, such as access to the opioid-reversal drug naloxone, and syringe exchange programs, which had long been rejected as too controversial.
Current Issue
The implementation of these “kinder, gentler” policies has been incredibly uneven. Plenty of white people who use opioids still suffer harms from prohibition markets and punitive policing. But the imperfect shift from carceral to a public health and health care approach has made a real difference in reducing the damage borne by white opioid users and their communities. In 2020, even as fentanyl continued to dominate the illicit market and drive up overdose rates, the rate of increase among Black individuals exceeded that for whites for the first time since 1999.
As always seems to be the case, however, it’s a very different story among Black and brown communities. People who use drugs from these communities have been largely excluded from the new health care approaches and are still forced to navigate criminalizing prohibition markets that have become even more dangerous with the entrance of xylazine, an animal tranquilizer that can extend the effects of fentanyl.
This is no accident. For decades public investment in Black and brown communities has been shifted from health care to punitive and militarized policing, leaving them with underfunded health care and harm reduction services crucial to survival amid increasingly potent and dangerous drug markets. As Diana Richardson, former New York State Assembly member representing Crown Heights, Brooklyn, said before the Assembly in 2016:
When there was a drug issue in the African American community, we were prosecuted. We were put in jail…. But now we have an opiate issue. It has affected another demographic. And now it is a health issue?
History offers a grim prediction of what will happen next. Authorities will eventually, if imperfectly, get a handle on the health crisis in white communities. The “whiteness” of the crisis will fade from public view and, soon enough, from public memory altogether. Left alone as the public face of the “drug crisis,” Black and brown consumers will be portrayed as a terrifying threat to the social order and will face a renewed racist Drug War–style crackdown.
How do we know this? Because it’s happened repeatedly in the past: For example, with opioids (including Bayer’s heroin) at the turn of the 20th century, and again with cocaine (powdered shifting to “crack”) in the 1970s and ’80s. If we want to stop it from happening again, all policies addressing drug-related harms need to be explicitly anti-racist, or else they will automatically become part of a century of segregated and failed drug policies—with health care for those categorized as white and “war” for everyone else.
In practice, this means transforming both sides of our Jim Crow drug policies. On the supply side, rather than punitive prohibition (which always disproportionately targets racialized communities), authorities need to focus on establishing robust consumer protections and ensuring safe supply. This means individual-level tools such as fentanyl test strips, but also structural reforms to ensure a robustly and intelligently regulated legal supply. On the demand side, we need to desegregate health care so that all people, including those who use drugs, have access to respectful and effective health care, as well as to the resources to meet the basic needs that drive health outcomes, including housing, food, and social support. These dedicated investments must focus especially on Black and brown communities in order to repair decades of disinvestment—or, more accurately, mis-investment in policing in those communities rather than in economic opportunity. Color-blind policies will not be sufficient; given the enormous imbalance of health care and social safety nets by race, relieving the now outsize acceleration of overdose deaths in Black and brown communities will require racially just redistribution of resources. And new policies should be reviewed in terms of their predicted effects by race. There is a clear model available in the EPA’s racial impact assessments. This is not a pipe dream: According to the Sentencing Project, nine states have already implemented laws calling for racial impact assessments of drug and other policies.
It’s not too late to fix our eyes on these goals and undo the damage of a century of “drug wars” waged against our own people. But to do so we need to recognize that our crisis is, and has been, as much about race as it has been about drugs.